January 2022
 By Chhavi Sodhi
By Chhavi Sodhi
Recently released findings from National Family Health Survey-5 (NFHS-5), 2019-’21 illustrate that the national contraceptive prevalence rate among married couples (15-49 years) has increased from 53.5 percent in 2015-16 to 66.7 percent in 2019, while the total fertility rate (TFR) has declined to 2.0, below the replacement level. This is a positive development, but the work on Family Planning (FP) in India is not done yet. It is imperative to reflect on whether and how these increases are related to greater reproductive autonomy and decision-making for women on the ground. Looking at the data deeper revealed that a whopping 43.6 percent of women in India (15-49 years) using a modern contraceptive for spacing discontinued their chosen method within 12 months of commencement and 5.7 per cent switched over to a newer method of choice (as per NFHS-4, 2015-’16).
Over the last two decades, increases in the variety and reach of contraceptive methods available within the family planning (FP) basket of choice in India have enabled more women and couples to gain access to different contraceptive methods catering to their specific fertility and health needs. Increasing the types of contraception available also increases the likelihood of choice to switch to and fro different methods. The concept of contraceptive switching is central to upholding the right to reproductive choice by women and enabling them to use contraceptives effectively. However, it is important to understand the basis of such decision-making and the experiences of women who orchestrate a sideways shift across methods.
Contraceptive switching, as the name implies, refers to the process of discontinuing a contraceptive method and adopting an alternate method (either permanent or temporary) within two months. Switching, here can be direct, wherein a woman shifts from one method to another sequentially or can be an uneven process. In the latter scenario, post-discontinuation, there can be a period of no use or the use of an intermediate method, before the woman settles on a particular destination method. There may also be an overlapping of methods before the final switch is made. In numerous instances, it has also been observed that women may come to accept contraceptive discontinuation, particularly if the period of no use becomes prolonged, thereby, switching from an earlier method of choice to no method.
Contraceptive discontinuation and switching rates in India
The use of a contraceptive method is not just mediated by its popularity and availability, but also by a series of decision-making events about adoption, discontinuation and rejection of other methods. Social, medical, systemic and personal factors can act, either in tandem or independently, to catalyze change. Due to a variety of these personal or social reasons, there may be a general dissatisfaction with the current method or there may even be a simple desire to try out an alternative method.
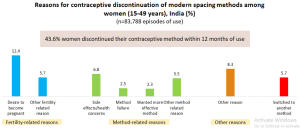
Source: National Family and Health Survey-4 (NFHS-4), 2015-’16: India
As per NFHS-4, 2015-’16, discontinuation rates were higher among women using injectables (50.6%), condoms (47.2%) and pills (41.9%), as compared to those using an intrauterine contraceptive device or IUD (26.4%). While 18.1 percent of all women using a modern spacing contraceptive stated that the reason they discontinued their earlier method of choice was due to fertility-related reasons, 17.1 percent claimed that they orchestrated this change due to method-related reasons, including failure of origin method (2.5%), experiencing side-effects from use of origin method (5.5%) and the desire to use a more effective method (2.3%). The data shows that 20 percent of women discontinued their earlier method of choice and switched to no method use, despite no explicit desire to beget children immediately. Given the situation, it becomes important to understand the method-specific barriers towards usage that constrain women and couples from exercising their reproductive rights and autonomy vis-à-vis contraceptive usage.
Well known reasons of discontinuation are spousal, familial and social pressures and lack of agency among women who wish to use contraceptives but face accessibility constraints; the role played by the health service system in supporting and responding to the concerns of women using or wanting to use contraceptives needs to be examined in greater depth.
How can the health system enable more informed contraceptive choices among women?
Findings from NFHS-4, 2015-’16 reveal that among users of female sterilization, oral pills and IUD, a total of 46.5 percent had been informed about the possible side effects of their method, while only 39.3 percent had been informed about ways in which these side-effects could be managed and 54.0 percent had received information about alternative methods available. Rana et al (2021) state that users with knowledge of alternate methods demonstrated a greater likelihood of switching, as the information enabled them to make a more informed contraceptive choice, in keeping with their contraceptive requirements. Similarly, information about side-effects and their management enabled women to make better choices about their destination method and continuing with the same. The latter was also associated with a shift towards the more efficacious long-acting reversible methods, including IUCD and injectables. In the absence of comprehensive knowledge about a new method of choice, including possible side-effects and their management, the authors mention probability of discarding the destination method and reusing or switching back to the original method remained considerably higher.
The health system, and in particular, contraceptive counseling, can play an important role in enabling a relatively smoother and desirable transition between contraceptive methods. In particular, women need additional support during the intermediate period of a transition, since the likelihood of an unintended pregnancy is particularly high during this period. Similarly, soon after the transition is made, they may need greater support and reassurance as they learn how to adapt to the mechanisms of a new method.
Evidence from NFHS is also pointing to a rise in the number of women who may be switching from modern to traditional methods, the use of which increased from 5.7 per cent in NFHS-4, 2015-’16 to 10.2 per cent in NFHS-5, 2019-’21. We need to understand whether this transition represents a way for women to exercise greater control over their bodies or has been an outcome of factors, both household or health-system related, that impeded their access to modern contraception. Understanding choice and agency in the context of contraceptive switching can be critical for ensuring that the FP services provided by the healthcare system addresses their needs.
How do we reframe the narrative on contraceptive switching?
The COVID-19 pandemic provides a more urgent reason to re-examine patterns of contraception use and switching that can be central to women’s reproductive autonomy. In the past two years, healthcare delivery in India has been severely compromised. During the numerous lockdowns and stay-at-home orders, people faced various restrictions not only on their movement but healthcare practitioners, including frontline workers (FLWs), too experienced a considerable increase in their daily work responsibilities, as they dealt with the aftermath of the disease. These factors have led to a de-prioritization of women’s health and FP needs. There was a decline in in-clinic consultations as well as a reduction in the availability of facility-based methods (female sterilization and intra-uterine contraceptive devices), which limited the basket of choices available and hindered the possibility of switching, while increasing the likelihood of discontinuation.
We need to better unpack reproductive autonomy in the context of India, particularly given contraceptive switching and discontinuation rates in India. The next phase of work for FP in India must include answering the questions below:
- Why do women switch or discontinue contraception, and how do the reasons vary across social groups?
- How does women’s access to contraception method specific information lead to a consciousness of choice?
- Who are the enablers of informed contraceptive choice among women, in the family and the health system, and how can enablers be influenced?
- What interventions and services by family planning programs can support the information and decision-making processes for making choice for a new method
- How can family planning counseling improve women’s choice and agency around switching and discontinuation
About the author:
Dr. Chhavi Sodhi, PhD (Social Medicine), is a trained public health professional with over five years of experience in monitoring and evaluation. She has worked in the field of RMNCH+A, nutrition, health system and environmental health research.
